Compliance 101: Medical Spa Policies and Procedures
.png)
Empowering Professionals at Every Stage
Portrait offers strategic expertise to help you make informed decisions and achieve long-term success.
Book Intro CallOperating a med spa in a complex healthcare ecosystem demands med spa owners to have a precise understanding of a multifaceted legal and regulatory framework, especially so if you’re a non-physician. It’s all about ensuring every aspect of your operation—from patient intake to service delivery and financial practices—adheres to compliance and health standards designed to protect patient safety, be at the forefront of their wellness journey, and maintain integrity.
Recent data shows that compliance violations are costly and increasingly common: fines for HIPAA breaches can exceed $2 million annually, and unauthorized practice of medicine or inadequate supervision can result in criminal charges, business closure, and license revocation for both clinics and supervising physicians (and other healthcare professionals), whether they’re on-site or in telemedicine. This also includes cosmetologists and estheticians, who execute more non-invasive procedures.
OSHA’s 2025 rules have raised the bar for sanitation and workplace safety, mandating rigorous infection control and employee protections. State laws further dictate ownership requirements, supervision protocols, and scope of practice—some requiring physician ownership, others permitting nurse practitioners or management service organizations (MSOs) to operate under physician oversight.
Laws that codify corporate practice of medicine (CPOM) also prohibits non-licensed entities from owning or controlling medical practices and from influencing medical decision-making. Lastly, advertising, medical recordkeeping, consent forms, and medical waste protocols are all under scrutiny, with enforcement and litigation on the rise.
Why is Compliance in Medical Spas Not Optional
Compliance in a medical spa setting is not an optional add-on; it is a foundational pillar of ethical and legally sound operations. Ignoring or underestimating its importance carries significant repercussions, impacting everything from your financial stability to your professional reputation.
Understanding why compliance is non-negotiable and recognizing the dynamic nature of its requirements is the first critical step toward safeguarding your practice. Primarily, it directly impacts patient safety. Medical spa procedures, while often aesthetic in nature, involve medical interventions that carry inherent risks.
Regulations ensure that these procedures are performed by qualified professionals with appropriate training, in appropriate settings, and with proper oversight, thereby minimizing potential harm to your clients. Failure to comply can lead to severe penalties, including hefty fines, suspension or revocation of licenses, and even criminal charges. Beyond legal repercussions, non-compliance erodes public trust and can lead to costly lawsuits.
A compliant medical spa signals professionalism, ethical practice, and a commitment to patient well-being, fostering a loyal client base and a sustainable business model. Conversely, a single compliance lapse can trigger negative consequences that are difficult, if not impossible, to reverse. Irreversible damage to your reputation.
Medical Spa Industry’s Changing Regulatory Environment
Medical spa regulation is not static; it is in constant flux, shaped by new medical technologies, emerging treatment modalities, and evolving public health concerns. What was permissible last year may be prohibited today, and new requirements can arise with little warning. This dynamic environment necessitates continuous monitoring and proactive adaptation.
Regulatory bodies frequently update guidelines, introduce new statutes, and refine enforcement priorities. For your medical spa, this means that a "set it and forget it" approach to compliance is inherently risky. You must establish mechanisms for staying informed about legislative changes at federal, state, and local levels.
Ignoring these shifts leaves your practice vulnerable to unintentional violations, which are treated with the same severity as intentional ones. Proactive engagement with professional associations and legal counsel specializing in medical spa law is crucial for keeping your practice aligned with current standards.
Key Regulatory Bodies and Jurisdictions Affecting Your Medical Spa
Understanding which regulatory bodies exert authority over your medical spa is important. Your practice is not governed by a single, monolithic set of rules; rather, it operates within a complex web of overlapping jurisdictions, each with specific requirements that must be met. In the U.S, medical spas must comply with:
Federal Regulations
At the federal level, several key regulations impact your medical spa. The Health Insurance Portability and Accountability Act (HIPAA) is perhaps the most prominent, governing the privacy and security of patient health information. Compliance with HIPAA is not optional, regardless of whether you accept insurance.
Federal Trade Commission (FTC) regulations also play a significant role, particularly concerning advertising and marketing claims, ensuring truthfulness and preventing deceptive practices. Meanwhile, the Food and Drug Administration (FDA) regulates the devices, drugs, and biologics used in your practice, dictating their approved uses, labeling, and safety standards.
Furthermore, federal labor laws, such as those enforced by the Occupational Safety and Health Administration (OSHA), ensure a safe working environment for your staff. Adhering to these federal mandates forms the baseline for all your compliance efforts, protecting both your patients and your employees.
State-Specific Regulations
The majority of direct oversight for medical spas occurs at the state level. Each state maintains its own medical board, nursing board, and possibly pharmacy boards, which dictate the scope of practice for various licensed professionals. These state boards define who can perform which procedures, under what level of supervision, and with what qualifications.
For instance, the rules regarding physician delegation of medical aesthetic procedures to nurses or physician assistants vary significantly from one state to another. State departments of health often set facility requirements, including sterilization protocols, waste disposal, and emergency preparedness.
Furthermore, state consumer protection laws often mirror federal advertising regulations but may impose additional strictures. You must thoroughly understand the specific statutes and administrative codes applicable in the state where your medical spa operates, as these often contain the most granular requirements for your daily operations. A failure to understand these nuances can lead to immediate and severe consequences, including license suspension or revocation.
Local Ordinances
Beyond federal and state regulations, your medical spa must also comply with local ordinances. These can include zoning laws, business licensing requirements, fire safety codes, and local health department regulations.
Zoning laws dictate where your medical spa can be located and the types of services it can offer within that zone. Business licenses and permits are required for legal operation within a specific municipality or county. Local health departments may conduct inspections related to sanitation, waste disposal, and infectious disease control, often complementing or expanding upon state requirements.
Fire safety codes, enforced by local fire marshals, ensure that your facility meets specific standards for exits, fire suppression systems, and occupant capacity. While often overlooked, non-compliance with local ordinances can result in operational shutdowns, fines, and delays in obtaining necessary permits, effectively halting your business.
Read more on American Med Spa Association (AmSpa).
How to Establish Robust Policies and Procedures
A strong foundation for lasting compliance in your medical spa begins with clear, comprehensive policies and procedures. These documents form the operational blueprint for your business, guiding every aspect of workflow to promote consistency, accountability, and alignment with regulatory requirements throughout your team. Well-crafted policies not only help prevent costly mistakes but also foster a culture of safety, professionalism, and continuous improvement.
1. Develop a Comprehensive Compliance Manual
A comprehensive compliance manual is an indispensable tool for your medical spa. This document should serve as the central repository for all your operational policies, ethical guidelines, and regulatory requirements. It must clearly outline the roles and responsibilities of every staff member concerning compliance, from the front desk to the medical director.
The manual should include sections on patient safety protocols, emergency procedures, HIPAA compliance, informed consent processes, and adverse event reporting. Furthermore, it should detail internal audit procedures, disciplinary actions for non-compliance, and protocols for updating policies.
Developing this manual is not a one-time task; it requires regular review, similar to medical records, and updates to reflect changes in regulations, technology, and best practices. A well-structured compliance manual empowers your staff with clear guidelines and demonstrates to regulatory bodies your commitment to a culture of compliance.
2. Define Scope of Practice for All Personnel
One of the most critical aspects of compliance is clearly defining the scope of practice for every professional working in your medical spa. This means meticulously outlining which specific procedures each licensed individual—whether a physician, nurse practitioner, registered nurse, physician assistant, or aesthetician—is legally authorized to perform, under what level of supervision, and using what specific techniques.
These definitions must align strictly with your state's medical practice act, nursing practice act, and other relevant professional licensing board regulations. For example, a registered nurse might be able to administer injectables under the direct supervision of a physician, but an aesthetician typically cannot.
Failure to adhere to these distinctions can lead to serious legal ramifications, including charges of practicing medicine without a license for the individual and the spa, and disciplinary action against the supervising physician. You must ensure that every staff member understands their individual limitations and responsibilities within their licensed scope.
3. Inform Consent Protocols
Patient autonomy and protection are central to medical ethics, and this is operationalized through robust informed consent protocols. Before any procedure is performed, you must ensure that your patients receive comprehensive information about the treatment, including its nature, purpose, potential benefits, known risks (both common and rare), alternative treatments, and the estimated cost.
This information must be presented in clear, understandable language, allowing the patient ample opportunity to ask questions. The consent process must be documented thoroughly, typically through a signed consent form that clearly demonstrates the patient's understanding and voluntary agreement.
For more invasive procedures, a cooling-off period might be advisable. It is not enough to simply have a patient sign a form; the conversation and comprehension are paramount. Inadequate informed consent leaves your medical spa vulnerable to medical malpractice claims and regulatory sanctions.
4. Ensure Patient Privacy and Data Security (HIPAA)
Protecting patient privacy and securing their health information is a non-negotiable federal mandate under HIPAA. Your medical spa, even if it does not bill insurance, handles Protected Health Information (PHI), which includes medical histories, other medical records, treatment plans, and billing information.
You must implement robust administrative, physical, and technical safeguards to protect this data. Administrative safeguards include developing written policies for PHI use and disclosure, training staff, and assigning a privacy officer. Physical safeguards involve securing your facility, workstations, and paper records. Technical safeguards encompass encryption, access controls, audit trails, and data backup for electronic health records.
Regular risk assessments are essential to identify vulnerabilities and ensure ongoing compliance. A breach of PHI can result in significant financial penalties, reputational damage, and loss of patient trust, underscoring the critical importance of a comprehensive HIPAA compliance program.
How to Staff and Supervise for Legitimate Practice
The qualifications, licensing, and ongoing professional development of your staff, coupled with appropriate medical oversight, are critical for maintaining legitimate practice and ensuring patient safety. These elements are highly scrutinized by regulatory bodies.
1. Physician Oversight and Delegation
The cornerstone of a compliant medical spa is appropriate physician oversight. In most states, medical aesthetic procedures are considered the practice of medicine and, as such, require the direct or indirect supervision of a licensed physician. The level of supervision required—whether direct (physician physically present), indirect (physician available by phone), or general (physician establishes protocols)—varies significantly by state and by the specific procedure being performed.
The physician must be adequately trained in the procedures being delegated and must be actively involved in the medical spa's operations, not merely an absentee signatory. They are ultimately responsible for the delegated actions of other licensed professionals. You must understand and meticulously adhere to your state's specific delegation rules to avoid allegations of the unlicensed practice of medicine or improper supervision.
2. Qualifications and Licensing for All Practitioners
Every individual performing services in your medical spa must possess the appropriate and current professional license for their role. This includes physicians, nurse practitioners, physician assistants, registered nurses, and licensed aestheticians.
Beyond initial licensure, you must verify that their licenses are active, in good standing, and without any disciplinary actions. This verification should be conducted upon hiring and regularly thereafter, typically annually.
It is also essential that their qualifications, including education and specialized training, align with the services they are authorized to provide. Using unlicensed personnel for medical procedures or allowing licensed staff to operate outside their scope are serious violations with severe legal and ethical consequences for both the individual and the medical spa.
3. Training and Continuing Education Requirements
Licensure alone is often insufficient for comprehensive compliance; ongoing training and continuing education are imperative. Medical aesthetic technologies and techniques evolve rapidly, and your staff must stay current.
Build a strong training program that covers not only the technical aspects of procedures but also patient safety protocols, emergency response, and compliance updates. Many professional licenses require specific hours of continuing education, and your spa should support and track these requirements for all staff.
Specialized training for new equipment or procedures, along with regular refreshers on foundational skills, ensures that your team maintains proficiency and adheres to the latest best practices. Documenting all training is crucial for demonstrating your commitment to competent practice during audits or investigations.
4. Designated Medical Director
For virtually every medical spa, the role of a designated Medical Director is indispensable. This individual, always a licensed physician, holds ultimate legal and clinical responsibility for the medical services provided within the spa. Their responsibilities typically include establishing and approving protocols for all medical treatments, ensuring appropriate supervision of other practitioners, overseeing patient selection criteria, managing adverse events, and maintaining quality assurance.
The Medical Director must have relevant experience and training in the aesthetic procedures offered and must be actively engaged in the medical spa's operations. Their presence and active leadership are critical not only for regulatory compliance but also for fostering a culture of clinical excellence and patient safety. Without a legitimately engaged Medical Director, your medical spa operates on precarious legal ground.
Service-Specific Compliance Considerations
Each service offered by your medical spa carries its own unique set of compliance considerations. A generic approach is insufficient; you must delve into the specific regulations governing each medical spa treatment to ensure full adherence.
This includes cosmetic procedures, aesthetic treatments, and more, just look at any medical spa menu! You’ll be able to list a bunch.
1. Injectables (Botox, Fillers)
Injectable neurotoxins (e.g., Botox, Xeomin, Dysport) and dermal fillers (e.g., Juvederm, Restylane) are prescription medications and medical devices, respectively. Their administration is highly regulated. You must ensure that these products are sourced only from legitimate, FDA-approved suppliers and stored according to manufacturer guidelines.
Only licensed medical professionals, typically physicians, nurse practitioners, or physician assistants, or registered nurses under appropriate physician supervision, are authorized to administer these. The specific delegation rules for these procedures vary significantly by state.
Comprehensive informed consent, detailing risks such such as bruising, swelling, allergic reactions, and rare but serious complications like vascular occlusion or vision loss, is absolutely mandatory. Additionally, precise documentation of product lot numbers, expiration dates, and quantities injected is crucial for patient safety and regulatory tracking.
2. Laser Treatments and IPL
Laser and Intense Pulsed Light (IPL) treatments, used for hair removal, skin rejuvenation, and pigment correction, involve powerful medical devices that can cause significant harm if misused. Regulations typically dictate who can operate these devices, often requiring specific training and certification beyond general licensure.
Some states restrict operation to physicians or physician extenders, while others allow properly trained registered nurses or even licensed aestheticians under strict supervision.
Maintenance and calibration of all laser and IPL devices are critical for safety and efficacy; you must adhere to manufacturer guidelines and keep meticulous service records. Eye protection for both the patient and the operator, along with detailed protocols for managing burns or other adverse reactions, are essential components of compliance for these services.
3. Chemical Peels and Advanced Skincare
Chemical peels, particularly those involving higher concentrations of acids, and other advanced skincare treatments like microneedling, blur the line between cosmetic and medical procedures. Regulations often differentiate between superficial peels, which aestheticians may perform, and medium or deep peels, which typically require a physician's or delegated medical professional's oversight.
The depth of penetration and the chemicals used dictate the regulatory classification. You must clearly define and train staff on the specific types and concentrations of peels they are authorized to apply. Similarly, microneedling, especially when performed with devices that penetrate deeply, often falls under the medical scope of practice and requires medical supervision. Comprehensive client consultation to assess skin type, conditions, and potential contraindications is essential for all advanced skincare.
4. IV Therapy and Vitamin Infusions
Intravenous (IV) therapy and vitamin infusions are direct medical interventions involving the administration of substances directly into a patient's bloodstream. These procedures are unequivocally within the scope of medical practice. They require a physician's order, medical oversight, and must be administered by a licensed professional qualified to perform venipuncture and manage potential adverse reactions (e.g., registered nurse, nurse practitioner, physician assistant, or physician).
Strict protocols for sterile technique, medication preparation, patient monitoring, and emergency response to anaphylaxis or other complications are non-negotiable. The sourcing and integrity of all infused substances, which are prescription drugs, must also comply with pharmacy regulations. Offering IV therapy without rigorous medical protocols and qualified personnel presents significant legal and patient safety risks.
5. Weight Loss Programs
Medical spa weight loss programs, especially those involving prescription medications (e.g., GLP-1 agonists, appetite suppressants), require comprehensive medical oversight. These programs must be run by a licensed physician or under their direct supervision, as they involve patient assessment, diagnosis, prescribing medication, and ongoing medical monitoring for side effects and efficacy.
Clear protocols are important to determine for patient eligibility, medical history review, baseline laboratory testing, dietary counseling, and regular follow-up appointments. Non-prescription weight loss products or supplements offered must comply with FDA regulations for dietary supplements and avoid any unsubstantiated health claims. Misrepresenting the efficacy or safety of weight loss interventions can lead to significant regulatory scrutiny and consumer complaints.
How to Maintain Transparency in Medical Spa Advertising and Marketing
The way you communicate about your medical spa services is subject to strict regulatory oversight. Honesty, accuracy, and transparency are not merely ethical guidelines but legal requirements, particularly in healthcare advertising.
1. Avoiding Misleading Claims
Your advertising and marketing materials must be truthful and cannot make misleading claims. This includes avoiding exaggerated promises of results, implying guaranteed outcomes, or using before-and-after photos that are not representative or have been digitally altered without clear disclosure. Claims about "permanent" results or "painless" procedures must be substantiated and carefully worded.
The Federal Trade Commission (FTC) and state consumer protection agencies actively monitor health-related advertising for deceptive practices. Misleading claims not only risk regulatory penalties but also erode patient trust and can lead to costly consumer lawsuits. Every promotional message should accurately reflect the services offered and their realistic potential outcomes.
2. Testimonials and Endorsements
While testimonials can be powerful marketing tools, their use is strictly regulated. You must ensure that any testimonials are truthful, accurately reflect the experiences of actual patients, and do not make claims that your services cannot generally achieve. If a patient receives compensation for their testimonial, this must be clearly disclosed.
Furthermore, if you engage influencers or other endorsers, their material connection to your medical spa (e.g., free services, payment) must be prominently disclosed in their posts. Both the FTC and state medical boards provide guidelines on the ethical and legal use of testimonials and endorsements in healthcare. Unsubstantiated or undisclosed paid endorsements can lead to fines and reputational damage.
3. Price Transparency and Fee Structures
Clarity in your pricing and fee structures is essential for both ethical practice and regulatory compliance. You must clearly communicate the cost of services, including any potential additional fees, before treatment begins. Hidden fees or unexpected charges can lead to patient dissatisfaction and regulatory complaints. For package deals or subscriptions, the terms and conditions must be clearly outlined.
While specific price advertising rules vary by state, some jurisdictions require healthcare providers to disclose price ranges for certain common procedures. Furthermore, if your medical spa bills insurance for any services, your billing practices must be fully transparent and align with coding and reimbursement regulations, preventing any accusations of fraud or overbilling.
4. Compliance with Social Media Guidelines
Social media platforms are powerful marketing channels, but they also present unique compliance challenges. Your social media presence must adhere to all the aforementioned advertising regulations regarding truthfulness and avoiding misleading claims.
Additionally, you must be acutely aware of HIPAA compliance on social media. Sharing patient photos or testimonials, even with consent, requires extreme caution to ensure no Protected Health Information (PHI) is disclosed.
Developing a clear social media policy for your staff, outlining what can and cannot be posted, is crucial. This includes guidelines on professional conduct, avoiding disparaging comments, and refraining from offering medical advice online. A single inappropriate post can trigger a privacy breach or lead to professional disciplinary action.
How to Meet Facility and Safety Requirements
The physical environment of your medical spa and the safety protocols governing its operations are critical components of compliance, directly impacting patient and staff well-being. Regulatory bodies scrutinize these areas rigorously.
1. Sterilization and Infection Control
Rigorous sterilization and infection control protocols are non-negotiable in any medical setting, including your medical spa. You must adhere to OSHA standards for bloodborne pathogens, ensuring proper handling of sharps, bodily fluids, and contaminated waste.
All instruments that penetrate the skin or contact mucous membranes must be sterilized according to current CDC guidelines, using validated methods such as autoclaving. Single-use items must never be reused.
You must have clear policies for hand hygiene, environmental cleaning, and disinfection of treatment surfaces. Regular training for all staff on these protocols, coupled with meticulous documentation of sterilization cycles and infection control practices, is essential to prevent the spread of infectious diseases and demonstrate compliance.
2. Emergency Preparedness and Response Plans
Your medical spa must have comprehensive emergency preparedness and response plans in place to address a range of potential incidents. This includes protocols for medical emergencies (e.g., anaphylaxis, cardiac events, adverse reactions to treatments), fire, natural disasters, and security threats.
Your plan should clearly define roles and responsibilities, evacuation routes, communication strategies, and the location of emergency equipment (e.g., AED, emergency medications). All staff must be regularly trained in these plans, including CPR and first aid. For medical emergencies, having a physician or qualified medical professional immediately available, along with a clearly defined transfer agreement to a higher level of care if needed, is important.
An effective emergency plan safeguards patients and staff and is a key expectation of regulatory bodies.
3. Waste Management and Disposal
Proper management and disposal of medical waste are critical for environmental protection, public health, and regulatory compliance. Your medical spa generates various types of waste, including sharps (needles, scalpels), biohazardous waste (blood-soaked materials), and pharmaceutical waste. You must adhere to federal (e.g., EPA), state, and local regulations for the segregation, storage, transport, and disposal of each waste stream.
This typically involves contracting with a licensed medical waste disposal company. Maintaining accurate records of waste manifests and training staff on proper waste handling procedures are essential. Improper waste disposal can lead to significant fines, environmental contamination, and health risks.
4. Equipment Maintenance and Calibration
The medical devices and equipment used in your medical spa must be regularly maintained, calibrated, and serviced according to manufacturer specifications. This includes lasers, IPL machines, microneedling devices, sterilization equipment, and any other diagnostic or therapeutic tools.
Maintaining detailed service logs, calibration records, and documentation of repairs is crucial. Malfunctioning or improperly calibrated equipment can lead to ineffective treatments, patient injury, and regulatory non-compliance. A proactive maintenance schedule not only ensures patient safety and optimal treatment outcomes but also extends the lifespan of your valuable assets and prevents costly downtime.
How to Achieve Financial Compliance in Billing, Coding, and Audits
While many medical spas primarily operate on a cash-pay model, robust financial compliance is still critical. For those that do bill insurance, the complexities multiply significantly, demanding strict adherence to billing, coding, and anti-fraud regulations.
1. Accurate Billing Practices
Accurate and transparent billing practices are foundational to financial compliance. For cash-pay services, this means clearly communicating all costs upfront, providing detailed receipts, and adhering to your stated fee schedules. Avoid any deceptive billing practices or hidden charges.
If your medical spa offers services that are billable to insurance, you must use correct CPT (Current Procedural Terminology) codes and ICD-10 (International Classification of Diseases, Tenth Revision) codes that accurately reflect the services rendered and the patient's diagnosis. Misrepresentation of services or upcoding (billing for a more expensive service than was provided) is a serious offense. Maintain records to support all billed services to ensure that the documentation justifies the charges.
2. Fraud, Waste, and Abuse Prevention
Prevention of fraud, waste, and abuse (FWA) is a critical compliance area, particularly for medical spas that interact with federal healthcare programs (even indirectly, if you prescribe medications covered by Medicare/Medicaid). Fraud involves intentional deception for financial gain. Waste involves incurring unnecessary costs due to deficient management or practices. Abuse involves practices that, directly or indirectly, result in unnecessary costs to the healthcare system.
Examples in a medical spa context could include billing for services not rendered, performing medically unnecessary procedures, or providing discounted services to generate referrals to billable procedures. You must implement a FWA prevention program that includes staff training, internal audits, and a mechanism for reporting suspicious activities. The consequences of FWA can be severe, including criminal charges, exclusion from federal healthcare programs, and substantial fines.
3. Manage Insurance Claims (if applicable)
If your medical spa provides services covered by health insurance, managing claims requires meticulous attention to detail. This involves accurate coding, timely submission of claims, and thorough documentation to justify the medical necessity of the services. You must understand the specific requirements of each insurance payer, including prior authorization processes, deductible and co-pay collection policies, and appeals procedures.
Furthermore, you must ensure that all services billed to insurance meet the definition of "medically necessary," as aesthetic procedures typically do not. Blurring the lines between cosmetic and medical services for the purpose of insurance reimbursement is a significant fraud risk. Robust internal controls and staff training are essential to navigate the complexities of insurance billing effectively.
4. Internal and External Audits
Regular internal and, where appropriate, external audits are vital for assessing and reinforcing financial compliance. Internal audits involve periodic reviews of your billing records, patient charts, and financial transactions to identify potential errors, inconsistencies, or areas of non-compliance.
These should be conducted by trained staff or an independent consultant. External audits may be conducted by government agencies, insurance payers, or independent third parties to verify compliance.
Proactive audits allow you to identify and correct issues before they escalate into major problems, demonstrating due diligence. Maintaining comprehensive documentation of all audit findings and corrective actions taken is crucial for demonstrating your commitment to continuous improvement in financial compliance.
How to Respond to a Compliance Breach or Investigation
Despite best efforts, a compliance breach or an investigation can occur. Your ability to respond swiftly, systematically, and ethically will profoundly influence the outcome. Proactive planning is key.
1. Develop an Incident Response Plan
A well-developed incident response plan is your blueprint for navigating a compliance breach or adverse event. This plan should clearly outline the steps to be taken when a potential violation is identified, including immediate actions to mitigate harm, who to notify internally and externally (e.g., legal counsel, regulatory bodies), and how to document the incident.
The plan should cover various scenarios, such as a patient privacy breach, an adverse event during a procedure, or an accusation of improper billing. Having a pre-defined process ensures that your response is organized, consistent, and compliant with reporting requirements, minimizing panic and potential missteps. Regular drills and staff training on the incident response plan are essential to ensure readiness.
2. Carry Out Internal Investigations and Corrective Actions
Upon discovery of a potential compliance breach, initiating a thorough internal investigation is crucial. This investigation must be objective, systematic, and documented. It involves gathering all relevant facts, interviewing involved personnel, and reviewing policies and procedures. The goal is to determine the root cause of the incident, assess its scope and impact, and identify individuals responsible.
Following the investigation, you must implement appropriate corrective actions. These could include revising policies, retraining staff, disciplinary action for employees, or making restitution. Demonstrating a proactive approach to identifying and rectifying issues is viewed favorably by regulatory bodies and helps prevent recurrence.
3. Cooperate with Regulatory Authorities
If your medical spa becomes the subject of a regulatory investigation by a state medical board, health department, or federal agency, full and transparent cooperation is paramount. This does not mean waiving your rights; rather, it means responding promptly to information requests, providing accurate documentation, and allowing reasonable access to your facility and personnel.
It is essential to engage legal counsel specializing in medical spa compliance immediately upon receiving notification of an investigation. Your attorney can guide you through the process, ensure your rights are protected, and help you present your case effectively. Obstruction or a non-cooperative stance can significantly worsen the outcome of an investigation, leading to more severe penalties.
4. Manage Reputation or PR During a Crisis
A compliance breach or regulatory investigation can severely damage your medical spa's reputation. Managing this crisis effectively requires a strategic and empathetic approach. While legal counsel will guide your communication strategy, generally, it involves communicating transparently and responsibly with affected patients, staff, and the public, as appropriate.
Focus on outlining the steps you are taking to address the issue, reinforce your commitment to patient safety and compliance, and express any necessary apologies. Avoid speculation or assigning blame publicly. Demonstrating accountability and a commitment to improvement can help rebuild trust over time. A PR professional specializing in crisis management may also be invaluable during such periods.
Proactive Strategies for Sustained Compliance
Compliance is not a destination but a continuous journey. To truly succeed, your medical spa must embed proactive strategies that ensure sustained adherence to regulations, adapting as the industry evolves.
1. Regular Risk Assessments and Gap Analyses
Regular risk assessments and gap analyses are indispensable tools for proactive compliance. A risk assessment identifies potential areas of non-compliance, vulnerabilities, and threats to patient safety or business operations. A gap analysis then compares your current policies and practices against regulatory requirements and industry best practices to identify "gaps" that need to be addressed.
These assessments should be conducted periodically, perhaps annually or bi-annually, and whenever significant changes occur in your services, equipment, or regulations. They allow you to prioritize compliance efforts, allocate resources effectively, and implement preventative measures before issues arise.
2. Hire a Compliance Officer
Designating a Compliance Officer, even if it's a part-time role for an existing senior staff member, signals a serious commitment to compliance. This individual is responsible for overseeing the development, implementation, and enforcement of your compliance program.
Their duties typically include staying abreast of regulatory changes, conducting internal audits, providing compliance training, managing the incident response plan, and serving as the primary point of contact for compliance questions. For larger medical spas, a dedicated full-time Compliance Officer is highly advisable. This centralized role ensures that compliance remains a continuous priority and is effectively managed across all facets of your operation.
2. Use Technology for Compliance Management
Leveraging technology can significantly enhance your compliance efforts. Electronic Health Record (EHR) systems with robust security features can assist with HIPAA compliance and accurate patient documentation. Practice management software can help track staff licensing, training, and equipment maintenance schedules, such as Portrait Care.
Compliance management platforms can also provide centralized repositories for policies, track regulatory updates, and automate internal audit processes. While technology is a tool and not a substitute for human oversight, it can streamline compliance tasks, improve data security, reduce manual errors, and provide real-time insights into your compliance posture, making your efforts more efficient and effective.
3. Continuous Monitoring and Adaptation
The regulatory environment is dynamic, meaning your compliance program cannot be static. Continuous monitoring of legislative and regulatory changes, industry trends, and internal performance metrics is essential. This involves subscribing to legal updates, participating in professional associations, and regularly reviewing your policies and procedures against current standards.
Your compliance program must be adaptive, allowing for prompt adjustments as new requirements emerge or as your practice evolves. This culture of continuous improvement ensures that your medical spa remains resilient, compliant, and prepared for future challenges and opportunities within the aesthetic healthcare landscape.
How to Keep Up with Medical Spa Regulation
The trajectory of medical spa regulation points towards increasing scrutiny and standardization. Understanding these trends will allow your practice to remain not just compliant, but ahead of the curve.
1. Anticipate Legislative Changes
The medical spa industry is experiencing rapid growth, which often attracts increased attention from lawmakers and regulatory bodies. As more complex medical procedures become mainstream in aesthetic settings, you can anticipate further legislative changes focused on enhancing patient safety, clarifying scope of practice, and tightening oversight.
These changes might include more stringent requirements for physician supervision, mandatory certifications for specific procedures, or expanded enforcement powers for state medical boards. Staying engaged with professional organizations and legal experts who monitor legislative developments is crucial.
Proactively anticipating these changes allows you to adapt your policies and training programs before new laws take effect, mitigating disruption to your operations.
2. Embrace Best Practices as the Industry Evolves
As the industry matures, the informal "best practices" of today often become the mandatory regulations of tomorrow. Embracing and implementing industry best practices, even those not yet codified into law, positions your medical spa as a leader in patient care and ethical operation. This includes adopting the latest evidence-based protocols for procedures, investing in advanced safety features for equipment, exceeding minimum training requirements, and fostering a culture of continuous quality improvement.
By consistently striving for excellence and operating at the highest possible standards, you not only elevate your own practice but also contribute to the overall professionalism and legitimacy of the medical spa industry, preparing your business for a future of even more rigorous oversight.
Build Your Medical Spa's Success with Portrait Care
Achieving and maintaining compliance in your medical spa is a comprehensive, ongoing commitment that underpins every facet of your success. Compliance isn’t just a legal obligation but a strategic move that safeguards patient well-being, protects your financial stability, and preserves your professional reputation.
By establishing proper policies and procedures, ensuring the right staffing and supervision, adhering to service-specific regulations, maintaining transparency in advertising, upholding stringent facility and safety standards, and practising diligent financial compliance, you create an unshakeable foundation for your practice.
What else? A platform to help you do all that will speed all these processes up. With Portrait Care, you’ll access technology, expertise, and proven marketing systems tailored specifically for med spas. You get to also tap into supply supplier savings of up to 60%. Talk to us today.
One Platform.
Everything You Need.
Everything You Need.
Portrait combines the technology, support, and savings to run and scale your modern medical wellness business.
Book Intro Call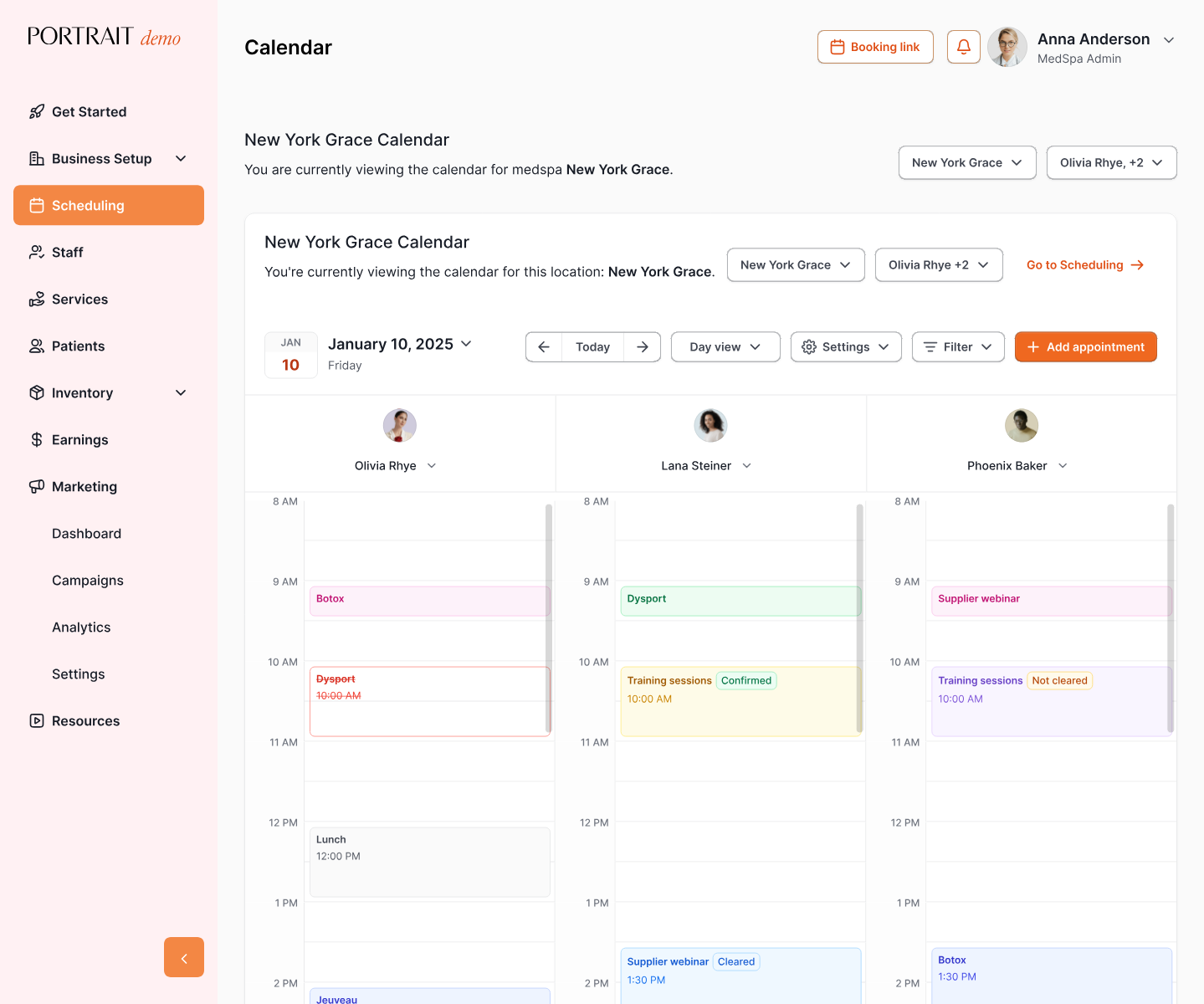
Stay Connected with Portrait Care
Subscribe to our email list and receive the latest insights, updates, and exclusive content delivered straight to your inbox.





